Arthritis and osteoarthritis negatively affect the patient's full life. When signs of the described joint lesions appear, people make hasty conclusions. They can make mistakes, confuse these pathologies. It is important to remember that the difference between arthritis and osteoarthritis of the knee is significant. Let's take a closer look at the characteristics of each disease. We will understand their differences, as well as how osteoarthritis differs from gonarthrosis of the knee joint.
Expand terminology
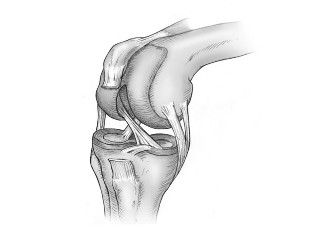
Arthritis and osteoarthritis are considered related words. Both mean joint damage. Due to the consonance of the terms, patients often perceive them as synonyms. This approach is wrong. To know how arthritis differs from osteoarthritis of the knee, you need to consider the characteristics of each.Osteoarthritis
Osteoarthritis is represented by deformity of the joints. The pathology is considered to be age-related. It is more common in elderly patients. It is also found in people under 40 years of age. More often its appearance is provoked by severe joint injuries, fractures. The risk group is represented by athletes. Read more about osteoarthritis of the knee.Arthritis
Arthritis is an inflammatory pathology that develops in a joint. It usually occurs by deteriorating the functioning of the relationship. The whole body is inflamed. The disease can flare up in any joint. It can also cover several connections at once. Learn more about knee arthritis.Difference between arthritis and osteoarthritis
The difference between arthritis and osteoarthritis is represented by the nuance that immune deficiency is considered a provocateur of inflammation. It can occur:
- Stressful situation; Hypothermia;
- Delayed flu.
Inflammation is provoked by an infectious agent, metabolic disorders and immune disorders. With the improved function of the body's defense system, the immune system works against itself.
Signs of arthritis
This pathology of the joints is manifested by the main signs and additional. The main ones are:
- Joint pain. It's strong, worse at night;
- Redness of the dermis over the affected joint, swelling.
There are additional signs of inflammatory disease:
- night pains, manifested with complete rest;
- pain relief when moving;
- morning stiffness. It passes in an hour;
- redness, swelling of the knees;
- attacks of severe pain in the knee. They last several days;
- the presence of dense nodules under the skin;
- subfebrile temperature;
- alternating swelling of the joints;
- blisters on the dermis, redness. They show the development of a reactive form of pathology;
- decreased appetite;
- weight loss.
Signs of osteoarthritis
The considered joint lesion proceeds with basic and additional signs. Among the main ones are:
- Crunching of the joints;
- localization in the knee area;
- restrict connection mobility;
- Pain is more common when moving. It rarely occurs at rest;
- joint deformity. Its appearance changes, the direction of the limbs may change;
- Deterioration of blood supply, nutrition of joint tissues.
Specific manifestations are:
- Onset of pain at night;
- attenuation of pain at rest;
- NSAIDs do not relieve pain;
- painful crisis;
- limited joint mobility; Osteophyte overgrowth.
Differences in major joint lesions
The key difference between osteoarthritis and arthritis is represented by the fact that osteoarthritis is a pathology of the joints that destroys and deforms it. Arthritis affects the functioning of internal organs. The kidneys, heart and liver suffer from this disease. When choosing a treatment, doctors pay special attention to the internal organs.
To make it easier to distinguish between diseases, we will illustrate them below.
| Signs of pathology | Osteoarthritis | ArthritisArthritisArthritis / zxtr>| Pain Syndrome |
Usually appears after moving. Pain is felt even after heavy loads. People do not pay enough attention, thinking that the pain provokes overexertion. The disease progresses and leads to painful sensations during light loads on the joint. The knees are also troublesome on rest days when the joint is not affected. In a comfortable position, the pain does not bother and subsides. |
In this pathology, the pain is felt all the time (during vigorous physical activity, at work, at rest). The disease is characterized by nocturnal pain, which is often bothersome from 3 to 5 in the morning. |
Crunch |
This is typical of this connection failure. Its appearance is provoked by the destruction of the cartilage layer, bone friction. At the same time, a specific sound (dry, harsh) is heard. It increases as the disease progresses. |
| Reduced joint mobility |
The affected joint reduces the range of motion. |
The joints, the whole body, are connected. |
Joint Deformity |
Appears gradually in the joints. If the disease aggravates the painful type of pain. There is usually no swelling. |
Deformation is also present. The area of the affected joint becomes red, swollen. Acute pain is felt after pressing. Possible nodes. The temperature at the site of inflammation rises. |
Blood test results |
Osteoarthritis does not tend to affect the result of blood tests. Inflammatory markers remain unchanged. |
This disease is characterized by an increase in ESR. An increase in the level of leukocytes indicates the course of inflammation in the joint. Biochemical analysis data show an increase in inflammatory markers. |
Localization |
Most often fixed in the knee joints. Less often, the disease affects the joints of the fingers, ankle. |
| |
Is there a difference between osteoarthritis and gonarthrosis of the knee joint? Gonarthrosis is an arthrosis that develops in the area of the knee joints. This pathology can be confused with a number of diseases:
- Meniscopathy.It is presented with damage to the menisci. This pathology, blockade of the knee joint can be observed in patients of different ages, of both sexes. In principle, a connection is subject to damage. The difference from gonarthrosis is the rapid development. Manifested by crunching, sharp pain in the joint after running, jumping, walking. After 10 - 15 minutes. pass sharp pain.
- Coxarthrosis(arthrosis of the hip joint). This diagnosis can be made due to the reflection of pain in the area from the hip joint to the knee. It is quite easy to distinguish such a condition. In coxarthrosis, the mobility of the knee joint does not change. It bends easily without pain. Doctors notice a decrease in the ability to rotate the leg "from the thigh". It is also difficult to stretch your legs to the side.
- Vascular painoccurring in the knee. The pain may indicate poor circulation in the articulated area of the knees. Such sensations are observed in adolescence. At this time there is active growth. Ships do not have time to develop as fast as bones. The pain in the pathology is symmetrical, it manifests itself equally in both limbs.
- Periarthritis. In inflammation of the tendons of the knee, the pain is felt after carrying heavy bags, after going down the stairs. The pathology is most often observed in women over 40 years. The pain does not extend to the entire knee. I felt only on the inner surface of my knees. The mobility of the knees is unlimited.
Differential diagnostics
With the described diseases of the joints, the doctor directs the patient to perform a differential diagnosis. It is important to distinguish between arthritis and osteoarthritis. There are also a number of subtypes of arthritis. Osteoarthritis occurs in several stages.
To distinguish these two pathologies from each other and from a number of other knee lesions, appoint:
- X-rays of compounds;
- blood biochemistry;
- rheumatic tests;
- CT;
- X-ray of the spine;
- NMR;
- bone scan.
Treatment of joint lesions
It is important to know what pathology you have been diagnosed with (osteoarthritis or arthritis of the knee joint) and not to be confused. Different approaches are used in the treatment of these diseases.
Medicines for the treatment of osteoarthritis

In the treatment of osteoarthritis, doctors use drugs (painkillers, hormonal drugs). they also use physiotherapy, therapeutic exercises, massage. If the case of pathology is particularly severe, drugs containing glucosamine sulfate are used. In some cases, surgery is required.
Therapeutic course for arthritis
Doctors choose a therapeutic course for arthritis, taking into account the form of the pathology. Patients should avoid strenuous exercise. exercise, excessive alcohol consumption, unhealthy diet. Therapy is carried out using drugs (non-steroidal anti-inflammatory drugs, antibiotics). In order to increase the effectiveness of the treatment, physiotherapeutic procedures and exercises are prescribed.
Prevention of joint pathologies
To prevent the development of pathologies such as osteoarthritis or arthritis of the knee joint, it is worth listening to the recommendations of specialists. As a precautionary measure, you must comply with the following requirements:
- Proper nutrition;
- Moderate exercise.

Each of these activities will be required even after treatment. Let's look at the characteristics of each of them.
Physical activity
They should be moderate. Such exercises contribute to weight loss, strengthen the corset of muscle fibers and increase blood circulation. Each element is very important for the prevention of joint diseases.
Heavy connection load
Patients should be careful. If you put an increased load on the joints, accidentally injuring them, you can get the opposite effect. Instead of improving the situation, new problems will appear. It is also dangerous to perform incorrect exercises from the exercise complex. All classes should be conducted under the supervision of an instructor, treating physician.
Gymnastics of the joints
As a preventive measure, it is enough to perform joint exercises. This is quite common. This is easy to do. In addition, you do not need to buy special equipment. Particular attention should be paid to exercises in the pool. When performing any activity in the water, the load on the joints is minimal.
Proper nutrition
Doctors recommend reviewing your diet, food preferences. For prevention, doctors recommend excluding a number of products from the daily menu. Among them:
- Red meat;
- Alcohol;
- Foods high in fat.
Must be included in the diet:
- Seafood;
- Fruit;
- fish;
- Gelatin (can be used as jelly meat, jelly dessert);
- Vegetables

Drink 2-3 liters of water a day. Alcohol is excluded. You need to start taking vitamins: calcium, D, B, A.
Other preventative measures are:
- Weight control;
- Protection against joint hypothermia;
- Mandatory maintenance of a healthy lifestyle;
- Proper sleep, rest;
- Wear comfortable shoes. It is possible to use shoes with orthopedic insoles, comfortable heels;
- Eliminate such a bad habit as crossing your legs while sitting;
- Eliminate stress.

















































